Testing for Vitamin A Poisoning – Liver Biopsy
There are several ways to test for vitamin A poisoning, some are better than others. Some tests are mostly useless, others likely also dangerous. There are also approaches I came up with.
I will present them one by one. Let’s start with what is considered to be the best.
A liver biopsy is considered the gold standard for vitamin A testing. During the test, an extracted tissue sample is analyzed visually. One can also directly measure the vitamin A concentration.
Liver Biopsy
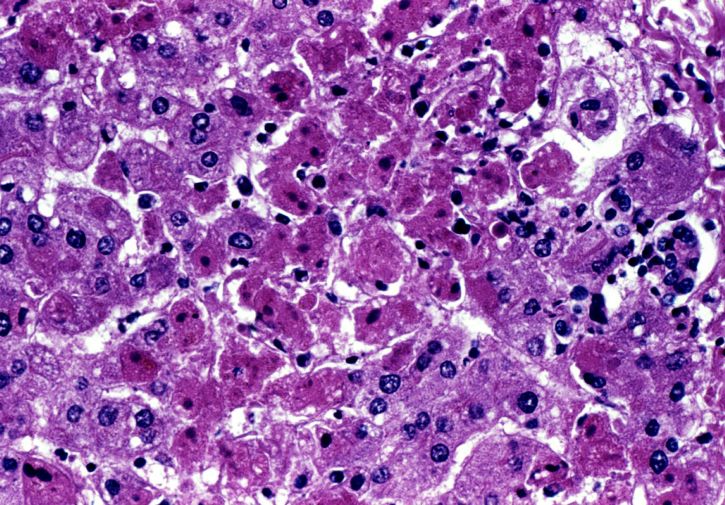
During a liver biopsy small parts of liver tissue are extracted from the patient and then examined under a microscope for liver damage associated with hypervitaminosis A. Vitamin A concentrations can be also directly measured in the liver tissue samples.
A liver biopsy is an invasive, minimally surgical procedure, that may require image guiding technology.
There are three different ways to perform a liver biopsy:
- Percutaneous (needle is inserted through the belly)
- Transjugular (through a vein in the neck, requires x-ray image guidance)
- Laparascopic (small abdominal incision)
What is examined during a liver biopsy:
- Direct measurement of vitamin A levels, ≧ 1.0 µmol VA/g liver is considered toxic. [1.0 µmol VA/g = 286 mcg/g = 286 mg/kg = 953 IU/g]. One source quoted ≧ 300 mcg/g as being toxic. The right lobe tends to have significantly higher vitamin A concentrations than the left lobe.
- Direct measurements of beta-carotenes [I don’t know the toxic levels, it’s possible there are none according to conventional understandings.]
- Light microscopic findings of increased number of lipid-laden hypertrophic stellate cells
- Electron microscopy for perisinusoidal fibrosis
- Ito cells (perisinusoidal lipocytes)
- Electron microscopy for lipid-laden hepatic stellate cells
- Dilated sinusoids (possibly the same as perisinusoidal lipocytes?)
- Vacuolated Kupffer cells
- Hepatocyte injury
- Fat-storing cell (FSC) hyperplasia
- Hypertrophy with indented nuclei and fluorescent vacuoles under ultraviolet (W) light microscopy
- Cirrhosis (scar tissue)
- Hepatitis (inflammation)
- Steatosis (abnormal retention of fat)
- Fibrosis (excessive fibrous tissue)
- Necrosis (dead cells)
- Peliosis (cystic blood-filled cavities)
What is often discussed in cases of hypervitaminosis A that were diagnosed via liver biopsy is the occurence of portal hypertension. This seems to be another strong indicator of vitamin A toxicity. It’s not clear to me whether it is something that is seen on the extracted tissue or something that is looked for at the same time when a liver biopsy is performed, without there being signs of it in the tissue samples.
Is a liver biopsy the best test for vitamin A diagnosis?
Although a liver biopsy is considered the gold standard for vitamin A toxicity and is the ultimate laboratory confirmation of poisoning, my research potentially calls this into question.
Looking at various studies and case reports over the past 60+ years, it appears that the microscopic examination for signs of liver damage or disease are more common nowadays than they were in the past. Often, there is no direct measurement of vitamin A levels in the tissue samples in recent case reports, only a visual examination.
This could potentially call into question the accuracy of liver biopsies as a diagnostic tool for vitamin A poisoning. If a diagnosis is mainly confirmed via visual interpretation of tissue samples, it appears that it would leave a wide room for error.
Risks
A liver biopsy carries a number of potentially serious risks:
- Pain
- Bleeding
- Infection
- Accidental injury to a nearby organ like the gallbladder or lung
- After a transjugular procedure: a collection of blood in the neck, injury to nerves in the face and eyes, voice problems, collapsed lung (pneumothorax), x-ray burden
My 2 cents
Personally, I would not do a liver biopsy. Or I would consider it only as a last resort. I have met too many incompetent doctors in my life to trust one of them with something that could potentially lead to organ damage.
The risk of that happening may be small, but I don’t see a sense in taking it, espeically since I can easily perform a test at home (through a low vitamin A diet trial) without anyone poking around in me.
It appears also that the way liver biopsies are examined these days is mostly microscopically. Meaning, the examining doctor looks for visual signs of liver damage. The vitamin A levels are not necessarily measured at all. This means that the accuracy of the test largely hinges on the competency of the pathologist. I have come across at least one case where Hypervitaminosis A was initially overlooked (but strongly suspected) and confirmed only after the tissue sample was examined a second time in a more rigorous fashion.
Note
Note, October 27th, 2023: This is an article that I originally published on my vitaminapoisoning.com website (now deleted).
Sources:
Liver Biopsy, Mayo Clinic website
Definition of hypervitamonisis A based on retinol levels found in tissue samples: “Nine subjects (33%) had hypervitaminosis A (≥1.0 μmol VA/g liver)”, mention of liver biopsies being the gold standard, 2018, Serum retinyl esters are positively correlated with analyzed total liver vitamin A reserves collected from US adults at time of death
Case report of hypervitamonisis A diagnosed via liver biopsy and detailed description of what was being looked at, 2016, Too Much of a Good Thing
41 cases of hypervitaminosis A, all confirmed via liver biopsies, 1991, Liver damage caused by therapeutic vitamin A administration: estimate of dose-related toxicity in 41 cases
Case report of hypervitaminosis A, 2006, Vitamin A toxicity: When one a day doesn’t keep the doctor away
“The vitamin A concentration is significantly higher in the right lobe than that in the left lobe” 1988, Vitamin A reserve of liver in health and coronary heart disease among ethnic groups in Singapore
“A liver biopsy was performed on the 16th hospital day. The hepatic vitamin A level was 3200 pg/g liver (normal <300) by the trifluoroacetic acid method (7).”, 1982, Hypervitaminosis A unmasked by acute viral hepatitis
Image:
Copyright Pixnio, Dr. J. Lyle Conrad, USCDCP
0 Comments