How Common Is Vitamin A Poisoning?

Contrary to popular belief, vitamin A poisoning appears to be a surprisingly common occurrence.
Based on liver biopsies conducted over the past 60 years, it has been found that vitamin A poisoning can affect up to 65% of the population.
You can find some of those studies further below.
This list largely builds on Dr. Garrett Smith’s presentation. (Although I have recalculated some of Dr. Smith’s numbers and arrived at slightly different percentages in some cases.)
Definiton of vitamin A poisoning
Retinol (vitamin A) can be measured in different ways and the results can be expressed in different units. Different studies use different units.
Vitamin A poisoning is confirmed during a liver biopsy at levels of above 1 umol/g.
> 1 umol/g = 286 mcg/g = 286 mg/kg = 953 IU/g
Those values are often rounded up to:
> 300 mcg/g = 300 ug/g = 300 mg/kg
> 1,000 IU/g
This refers to the amount of vitamin A per gram (or kg) of examined liver tissue.
Liver biopsy studies show widespread chronic vitamin A poisoning
Here is a list of studies that have examined the vitamin A levels in livers of human cadavers via a liver biopsy (the only reliable test to determine retinol content).
(1) 33% positive for vitamin A poisoning, USA, 2018
27 different cadavers were examined. Nine of them showed retinol levels above 1 umol/g.
“Nine subjects (33%) had hypervitaminosis A (≥1.0 μmol VA/g liver)“
The study was performed in the US and published in 2018.
Source: “Serum retinyl esters are positively correlated with analyzed total liver vitamin A reserves collected from US adults at time of death” (full text)
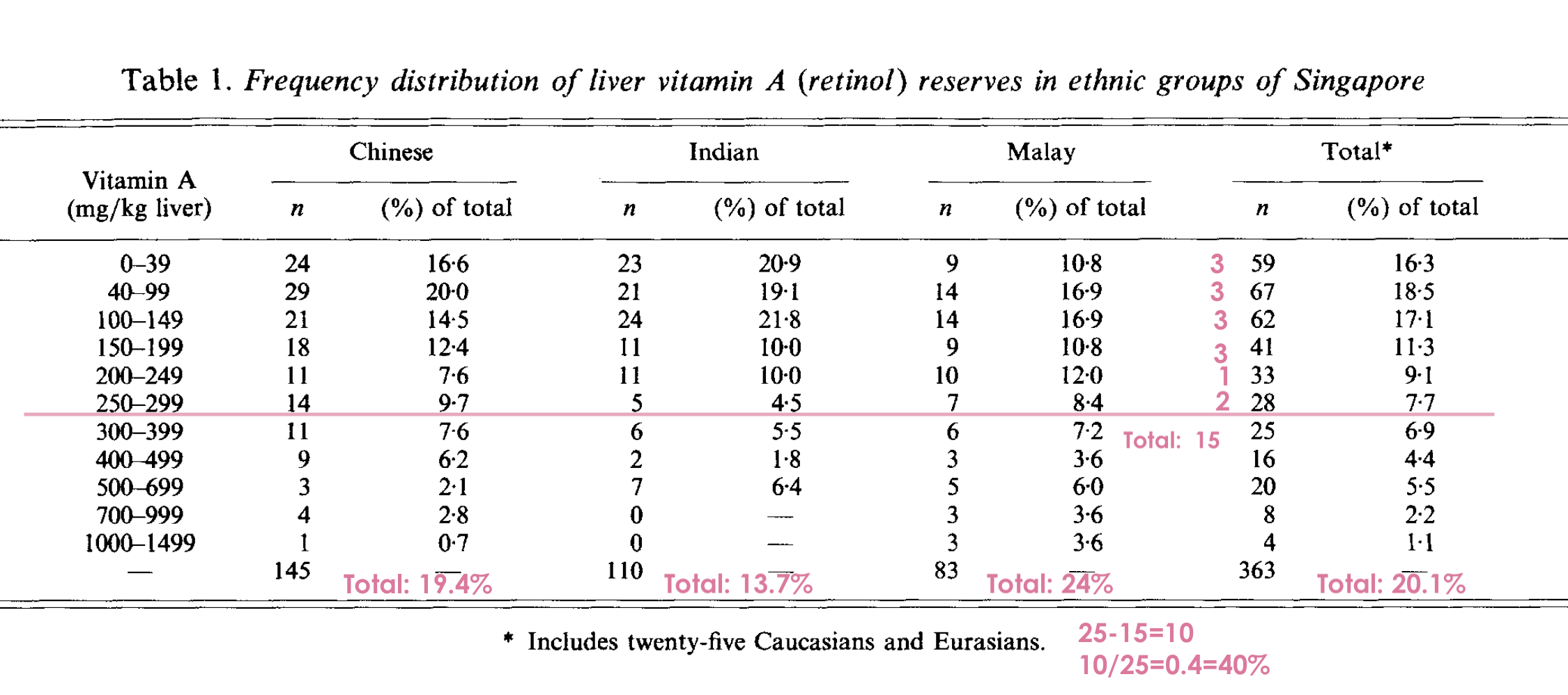
(2) 13.7% to 40% positive for vitamin A poisoning, Singapore, 1988
363 different tissue samples of Singaporeans of different ethnicities were examined.
Results:
- 13.7% of Indian Singaporeans
- 19.4% of Chinese Singaporeans
- 24% of Malay Singaporeans
- 40% of Caucasian and Eurasian Singaporeans
were shown to have hypervitaminosis A (levels of over 300 mg vit A/ kg liver).
10% had vit A levels of over 500 mg/kg:
”At the extreme end of the range, 9% of the subjects had concentrations above 500 mg/kg and 1 % of the subjects had concentrations above 1000 mg vitamin A/kg in the liver.”
Interestingly, there were also a number of individuals who had a retinol value of 0 mg/kg in the liver. Those were taken from healthy accident victims. Did anyone try to find out how they were doing before they died? Was their eyesight heavily impaired? Were they of extremely poor health? What symptoms did they have? If none, how does this fit the idea that vitamin A deficiency is a serious condition that needs fixing? Or are the zero values possibly a result of a laboratory error? Surprisingly, no one seems to have followed up on this issue, neither in this nor any other study.
Source: “Vitamin A reserve of liver in health and coronary heart disease among ethnic groups in Singapore”
Values above 300 mg of vitamin A per kg meet the criteria of vitamin A poisoning.
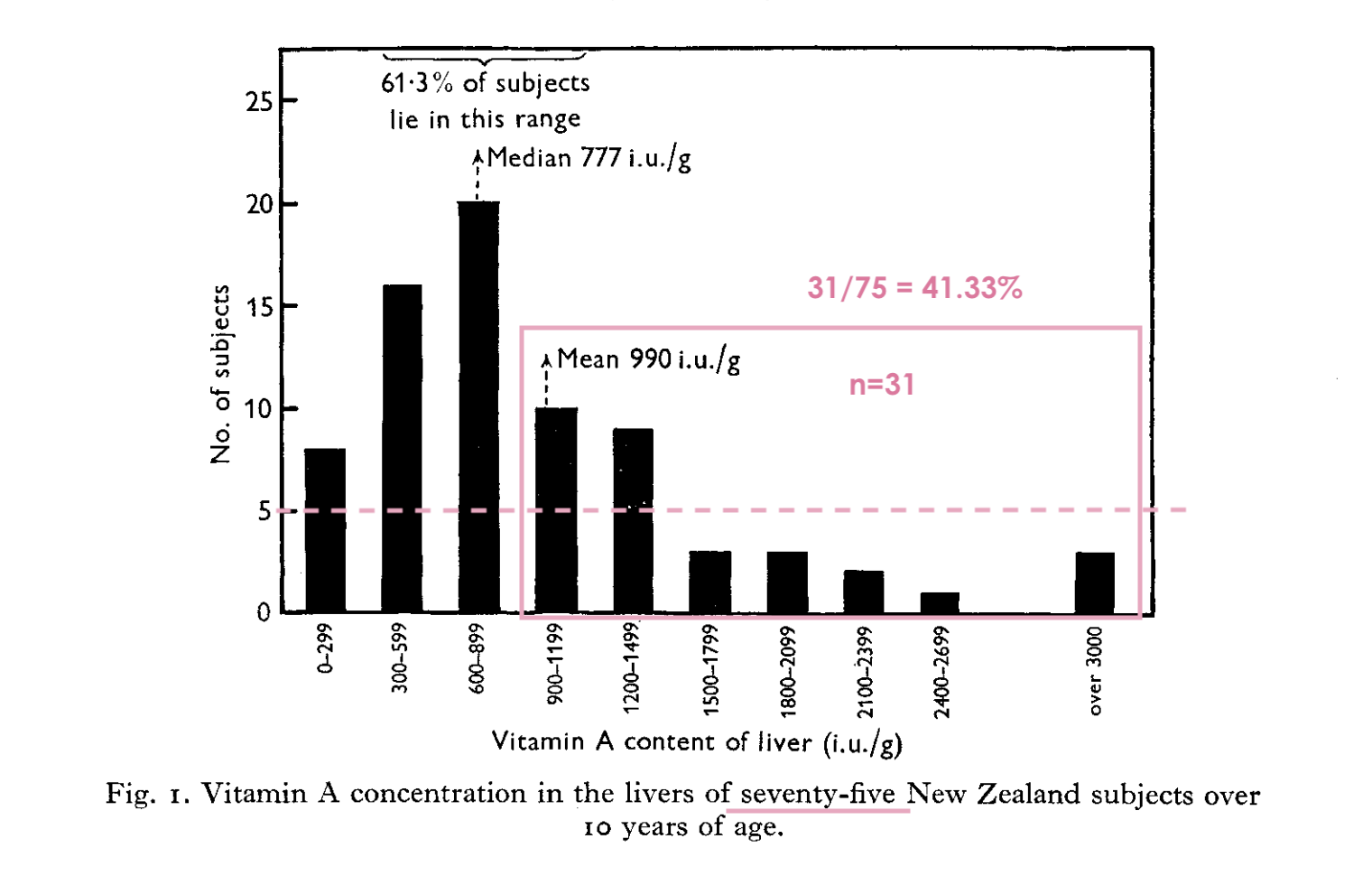
(3) 23% to 41% positive for vitamin A poisoning, New Zealand, 1951, 1960-61
The results of this study have been presented in a rather chaotic way, hence it is not clear what the correct percentage is that met the criteria of vitamin A poisoning.
But it’s either a minimum of 23.4% or as high as 41.3%.
The text says that a total of 111 samples from as many cadavers were collected, but the graph with the results depicts only 75.
Another problem: Vitamin A poisoning is defined with values of above 1,000 IU/g, but there is no range which starts with this value in the graph with the results. The relevant bracket starts with 900 IU/g.
If all the results (10) in that bracket (900 – 1,199 IU/g) are counted as positive for vitamin A poisoning group, then the total of those cases would be 31.
If we were to approach it conservatively, and say that only half of that bracket (5) is counted as positive for vitamin A poisoning, then the total would be 26 cases.
Consequently, the results would be:
If all 111 samples are considered, this would mean that 31/111 or 27.9% met the definition of vitamin A poisoning. If one chooses the conservative estimation and calculates with 26 total cases, then the percentage drops to 26/111 = 23.4%.
If only 75 samples are considered, then this jumps to 31/75, or 41.3% who met the definition of vitamin A poisoning. Or 26/75 = 34.7%.
So, I believe that a minimum of 23.4% and a maximum of 41.3% of the samples tested positive for vitamin A poisoning.
Source: “Vitamin A content of human liver from autopsies in New Zealand”
The study text mentions 111 samples, but strangely, only 75 are included in the graph with the results.
(4) 49% positive for vitamin A poisoning, Ghana, 1963
49 liver samples were examined. 24 of them had vitamin A levels above 300 ug/g, which meets the criteria for vitamin A poisoning. That’s nearly half, or 49%.
“The vitamin-A content of the forty-nine livers varied considerably-from 32 ug. per g. to 3635 ug. Twenty-four of the livers showed vitamin-A levels above 300 ug. per g. (…)”
Source: “HYPERCAROTENÆMIA IN GHANAIANS”
(5) 65% positive for vitamin A poisoning, Ghana, 1967
17 liver samples were examined from diseased people. 11 of them had vitamin A levels above 300 ug/g. That’s 65%.
Source: “Distribution of carotene and vitamin A in liver, pancreas and body fat of Ghanaians”
The results are presented in ug/100 g, so to get to ug/g, they need to be divided by 100. All the results which exceed 300 ug/g (or 30,000 ug/100g) and so meet the criteria for vitamin A poisoning are marked in pink.
(6) Around 4.9% to 21.9% positive for vitamin A poisoning, Canada, 1969
467 liver samples were collected in different Canadian cities (Halifax, Montreal, Ottawa, Winnipeg, Vancouver).
Between 4.9% and 21.9% were in the highest bracket of above 240 ug/g. Vitamin A toxicity is defined as values of above 300 ug/g. Unfortunately, the study did not include such a range. So, the actual percentage of vitamin A toxic individuals was likely slightly less than the above numbers.
Since vitamin A toxicity is defined as values of above 300 ug/g, the real percentage of vitamin A poisoned individuals was likely slightly lower than the ones in the highest bracket which starts at 240 ug/g.
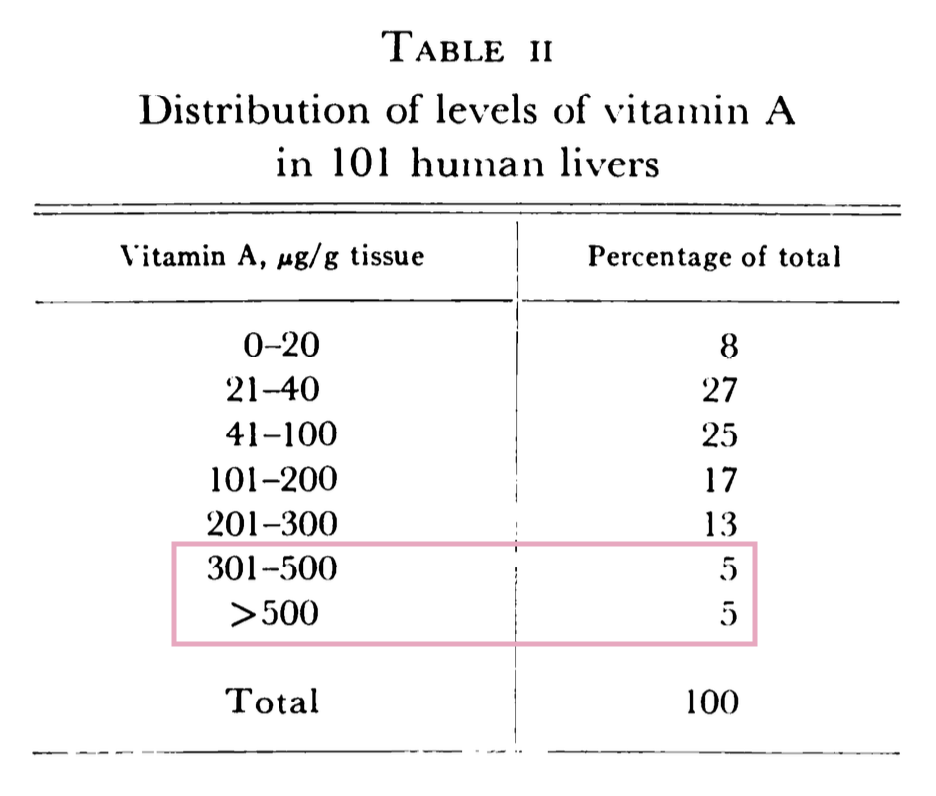
(7) 10% positive for vitamin A poisoning, USA, 1970
100 liver samples were examined. 10 of them met the definition of vitamin A poisoning of above 300 ug/g.
10 out of 100 – that’s 10%.
(8) 24,2% positive for vitamin A poisoning, USA, 1973
329 liver samples from dead people were collected and analyzed. 24.2% met the criteria for vitamin A poisoning of above 300 ug/g.
Source: “Vitamin A and carotene levels of a selected population in metropolitan Washington, D. C.”
24.2% out of 329 subjects in Washington D.C. turned out to be vitamin A poisoned in 1973.
(9) 31% positive for vitamin A poisoning, UK, 1982
364 liver samples were examined, 30.9% were above 300 mg/kg.
Source: “A survey of human liver reserves of retinol in London”
Nearly 31% of examined Londoners met the definition of vitamin A toxicity in 1982.
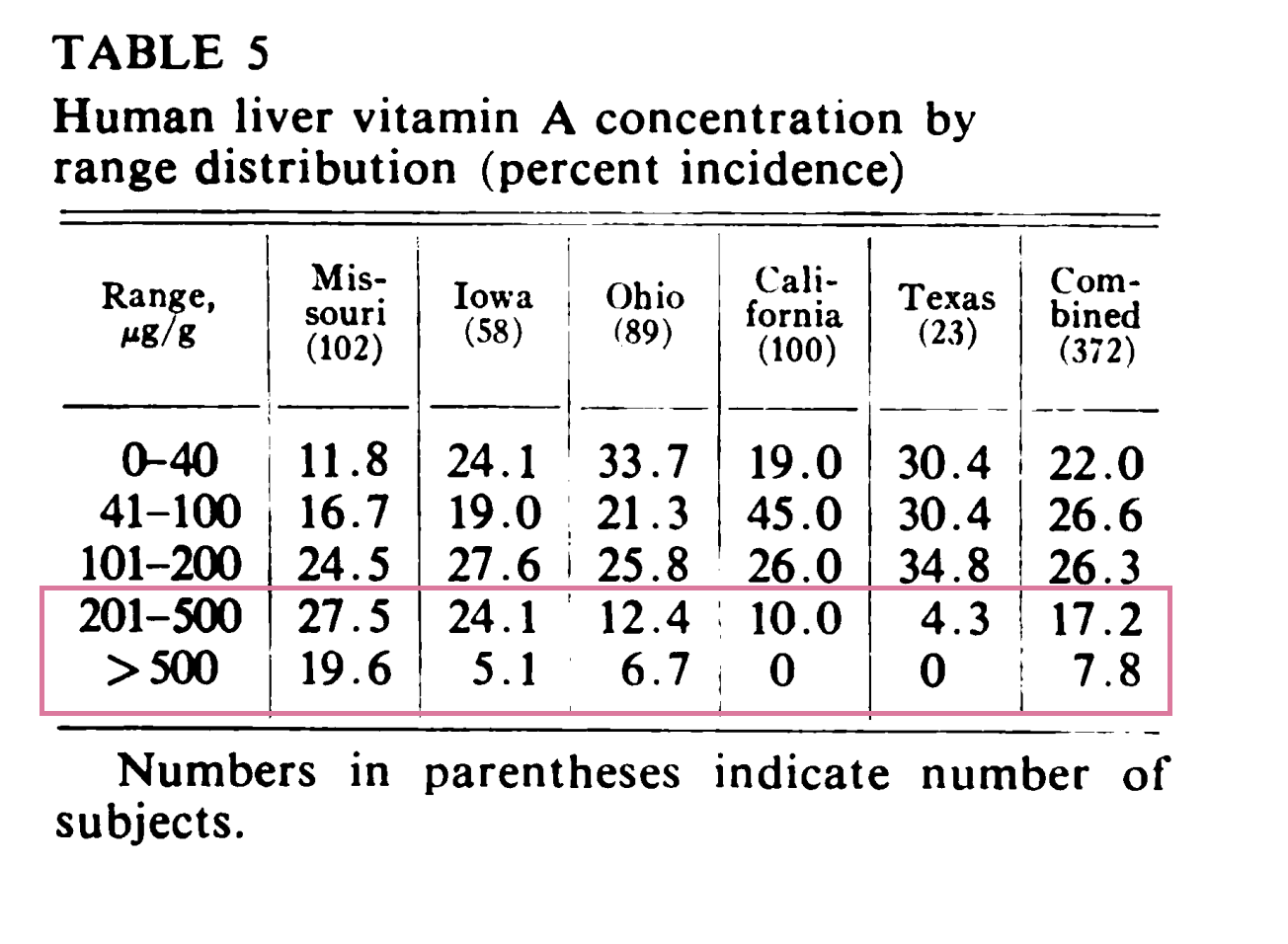
(10) Around 20% positive for vitamin A poisoning, USA, 1972
364 liver samples were examined, 30.9% were above 300 mg/kg.
Source: “Vitamin A concentration in human tissues collected from five areas in the United States“
Vitamin A toxicity starts at 300 ug/g. Unfortunately, the above table did not have such a range. So, it is not clear how many individuals in the 201-500 ug/g bracket were above 300 ug/g. But it is probably not far-fetched to assume that the combined average of individuals above 300 ug/g. was at around 20%.
Picture credit:
Pixabay: https://pixabay.com/photos/carrots-basket-vegetables-market-673184/
Copyright: jackmac34




The high prevalence of vitamin A poisoning in Ghana is interesting given how we hear so often of vitamin A deficiency in Africa. My understanding is that there is a lot of research in Africa and India showing vitamin A “deficiency” (meaning low serum retinol) correcting immediately with increased dietary zinc and protein. Without adequate production of Serum Retinol Binding Protein, the retinol never leaves the liver and builds up into a toxic state. It is well-known that African and Indian populations are often protein malnourished due to lack of meat consumption. Diets are often high carotenoids such as starchy orange root vegetables.